Pregnancy is an incredible time in any woman’s life. Whether your pregnancy is planned or a big surprise, you’re creating new life inside of you and that’s pretty amazing. Every woman’s journey through pregnancy is very unique, but I wanted to touch on a condition that affects 10% of pregnancies: Gestational Diabetes.
This post is for anyone who has been diagnosed with Gestational Diabetes (GD), has a spouse/significant other with GD, or is thinking of becoming pregnant and want to prevent GD. This post will be the first in a series to help you better understand what’s happening in your body when you have GD and how you can still have a healthy and uncomplicated pregnancy despite this diagnosis.
So let’s get started!
What is Gestational Diabetes?
Gestational Diabetes is simply high blood sugars that develop during pregnancy in women who previously never had high blood sugars. It is very natural during pregnancy to have increased insulin resistance and therefore, high blood sugars. Insulin is the hormone produced by the pancreas in response to elevated blood sugars to help transport glucose (aka sugar) after a meal from your bloodstream into the cells of your body to be used as an energy source.
What causes GD?
Like most health conditions, it is hard to say EXACTLY what causes GD. Some of the most common risk factors include:
- Family history of GD or Type 2 Diabetes
- Overweight at conception
- Age 25 years or older
- Non-Caucasian
- Previous large baby (greater than 8 lb 13 oz)
So you’re probably thinking now, EVERYTHING is a risk factor for GD! And you’d be right. Therefore, if you are diagnosed with GD, stop blaming yourself! You still have tons of potential and opportunity to have a perfectly healthy pregnancy despite the diagnosis of GD.
First Steps
Know Your Numbers
Alright, so now that we know what GD is and how it was potentially caused, where do we go from here? The first step is to monitor what exactly YOUR blood sugars are reading throughout the day. We do this by a finger-stick blood sugar check using a glucometer.
A glucometer is typically ordered by your doctor and *hopefully* you will get the chance to meet with a nurse, dietitian, or diabetes educator to show you how to use it in person. If you have not had the opportunity, most glucometer companies have excellent websites you can go to for video tutorials on using their meters, test strips, and lancing devices (the thing you use to poke your finger).
Every doctor is different, but most will ask you to check your blood sugar four times per day: fasting (first thing in the morning before any food or beverage besides water) and 1-2 hours after every meal. Once you start checking your blood sugars, you can see how close you are to the recommended blood sugar targets and adjust your diet and exercise accordingly.
Blood Sugar Goals (American Diabetes Association Guidelines):
Fasting: less than 95 mg/dl
1 hour after meals: less than 140 mg/dl
2 hours after meals: less than 120 mg/dl
It’s a great idea to keep a logbook of your blood sugars to take with you to every doctor’s appointment. I love the “pen to paper” logbook because you can see all your blood sugars for a specific time (example: fasting) on one page to observe trends. Your blood sugars will be stored in the meter if you forget to write them down.
Depending on the meter you’re using, it may have an app that you can connect to via Bluetooth to keep an electronic logbook. Other apps like mySugr can help track blood sugars, food, and medications all in one place.
Nutrition for a Healthy GD Pregnancy
Now that you have a glucometer and are checking your blood sugars, you’re ready to learn more about what effects those numbers. Our diet has the biggest impact on our blood sugars because when we eat foods containing carbohydrates (aka carbs), our digestive system breaks down those carbs into glucose which raise our blood sugar.
Foods that contain carbohydrates include: grains (cereals, breads, pastas, rice), starchy vegetables (beans, potatoes, corn, green peas), fruit, and dairy products (yogurt, milk). These are the foods we’ll be focusing on the most since they’ll have the biggest impact on our blood sugars.
Other foods that mainly contain fats and protein have little impact on our blood sugars: animal proteins (beef, chicken, pork, fish, eggs), nuts, seeds, butter, oils, avocados, cheese, and cream. These foods will be staples in a GD meal plan to help provide necessary nutrients and promote satiety (aka feeling full and not hangry!).
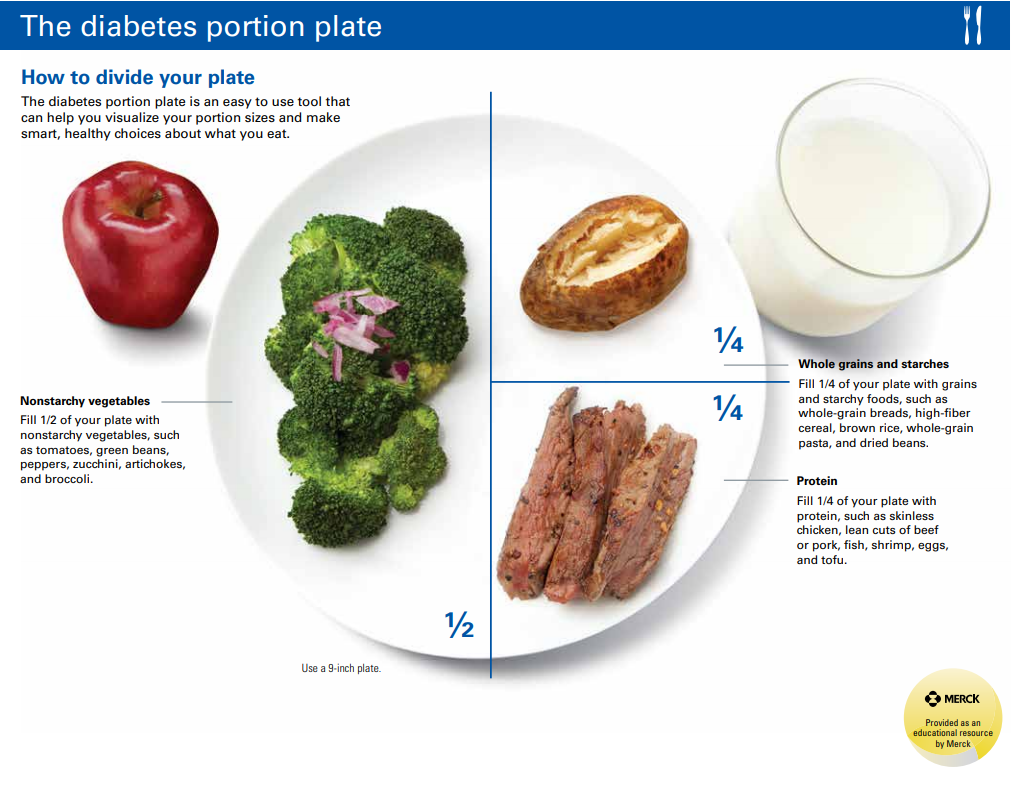
We’ll talk more in a future post about how to build and modify a healthy meal plan based around your personal blood sugars, but for now this visual below is a great start.
Try to include almost half your plate with non-starchy vegetables. These particular vegetables pack a punch with the vitamins and minerals you need during pregnancy, but they also happen to be low in carbohydrates so they won’t affect your blood sugars much. Fruit provides some important vitamins and minerals as well but they contain mainly carbs and no fat or protein so we want to be careful with the amount we consume.
¼ of of the plate is protein to provide you and your baby with the necessary amino acids (the building blocks of protein) for bone and muscle development. The remaining ¼ of the plate is for higher carbohydrate foods such as grains, beans, and starchy vegetables. This section can be modified as well depending on your blood sugars.
Dairy is also pictured alongside the plate and can vary in carbohydrate content. Cheese and cream are mainly sources of fat and protein and will not raise your blood sugars. However, milk and yogurt contain more carbs and may need to be included at snacks instead of meals.
Healthy fats, although not pictured above, should be included at every meal for your satiety and your baby’s brain development. Sources of healthy fats include: nuts, nut butters with no added oils or sugar, unsweetened coconut products, chia seeds, flax seeds, sunflower seeds, avocados/avocado oil, olives/olive oil, butter and ghee from pastured animals, salad dressings with a short ingredient list and free of added sugars, mayonnaise made from avocado oil, and heavy cream.
In future posts I will go into even more detail about how to modify your diet based on your blood sugars.
Additional Resources
Hopefully this post was able to provide you with some answers to your Gestational Diabetes questions. I will go into more details in future posts on nutrition during GD, nutrients of concern and supplementation, and what to do after pregnancy.
If you want to learn EVEN MORE about GD or nutrition during pregnancy in general, I highly recommend the following books:
Real Food for Pregnancy by Lily Nichols, RDN, CDE, CLT
Real Food for Gestational Diabetes by Lily Nichols, RDN, CDE, CLT
Please comment below with any questions you still have for future blog posts related to GD or pregnancy in general!
Follow me on social media and never miss a new post!
This post contains affiliate links, which means I receive a percentage of the sale if you use the link to make your purchase. This will not change the price of the product, but your support will help directly offsets the cost of web hosting and maintenance and is greatly appreciated!





Leave A Reply