Welcome back to the Gestational Diabetes series! If you haven’t read part 1 of the series go ahead and CLICK HERE. Part one gives you some foundational knowledge about what gestational diabetes is and where to get started.
Now that you’re up to speed on what gestational diabetes is we can get more detailed about to how to manage your blood sugars during your pregnancy with real food!
Gestational Diabetes (GD) is often described as a carbohydrate intolerance due to the insulin resistance women experience during pregnancy. Therefore carbohydrates will be our main focus of today’s blog post. Carbohydrates (carbs) are our bodies main energy source and remain very important despite a diagnosis of gestational diabetes.
My goal today is to make sure that you’re not afraid of any foods, especially carbs. I want you to understand that food is not the enemy and you can use food as medicine to help bring about the healthiest pregnancy possible.
Quick Recap: What are Carbohydrates?
Carbohydrates are the body’s main energy source and are found in grains such as pasta, rice, breads, cereals, fruits, dairy products, and starchy vegetables. There are little to no carbs in non-starchy vegetables, proteins, and fats. The goal here is not to completely eliminate carbohydrates from your diet, just to have them in small, controlled amounts evenly spread throughout the day to prevent large spikes in blood sugar.
It’s also not a good idea to eat “naked” carbs; aka carbs by themselves. Pair you carbs (such as fruit) alongside protein and healthy fats (such as nuts) to keep your blood sugar from rising and crashing quickly.
Meal planning
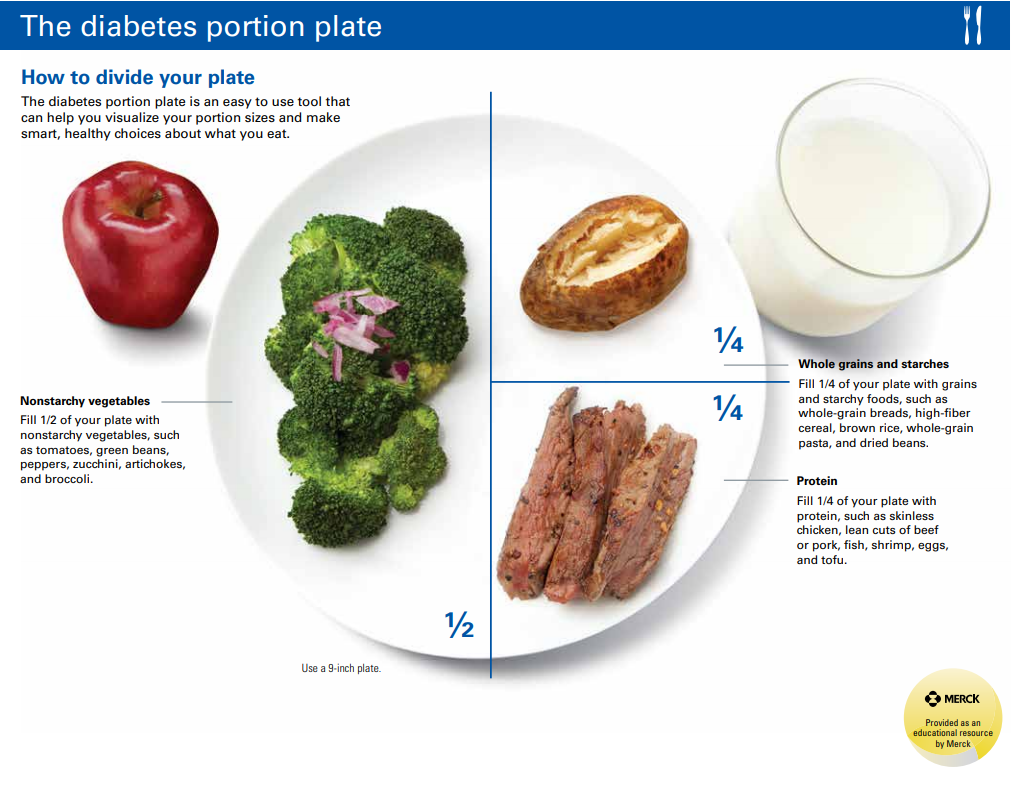
I briefly introduce the Portion Plate as a method of controlling carbs in my previous blog post. If tracking the grams of carbs you are consuming gets confusing, or if you are often in situations where carb counting is difficult, such as eating out at restaurants or family gatherings, feel free to use the plate method as a form of carbohydrate tracking.
I highly recommend using apps such as MyFitnessPal or Mysugr when starting to track your carb intake. When using apps, you have the carbohydrate information for restaurant foods, fresh produce, packaged foods, and common home-cooked meals at your fingertips. Most women don’t have to track their food intake the entire pregnancy. After 2 weeks you’ll have learned a lot about which foods are best for your blood sugars and you can eat more intuitively.
Every woman’s carb intake will be different and may change throughout the remaining weeks of pregnancy, so be flexible and don’t feel locked into a certain number of grams of carbohydrates. The exact amount of carbs you need at each meal can be highly individualized based on your post meal blood sugars. A good starting point is 30-45 grams of total carbohydrates per meal and 0-15 grams of total carbohydrates per snack.
Breakfast
One exception to this is breakfast. In the morning, it is natural during pregnancy to have more insulin resistance due to increased levels of cortisol. Therefore, some women benefit from keeping total carbs to 30 grams of carbs or less at breakfast and avoiding fruit and dairy products. Low sugar fruits such as berries and higher fat/protein dairy such as Greek yogurt, cheese, and cream may be tolerated just fine.
The process of individualizing your carbohydrate needs is why one of the first steps after being diagnosed with GD is to start checking your blood sugars. It’s the best way that you can individualize your meal plan and make sure that you don’t overly restrict your carbohydrates.
Evening Snacks
I usually recommend patients start with three meals per day and one evening snack. Your evening snack can be an important tool for preventing elevated blood sugars the next morning.
Elevated fasting blood sugars can occur for a number of reasons. The first being you had too many carbs at your evening meal and blood sugars are remaining elevated throughout the night. If this is the case, try reducing your carbs at dinner and adding an evening snack of 15 grams of carbs alongside a source of protein and fat. Remember, no “naked” carbs!
The second reason for elevated fasting blood sugars is that you skipped your evening snack. As crazy as it sounds, you can have high blood sugars the next morning by not eating! That’s because your liver stores an extra supply of glucose for emergencies. If you tend to go more than 10 hours without eating (say you skip your evening snack and get a full 8 hours of sleep), your liver may view this as an “emergency” and start releasing glucose into the bloodstream. Now if we would have just had an evening snack to begin with, we could eliminate this “emergency” response by the liver.
For a whole list of #Dietitianapproved Snacks CLICK HERE!
Making Adjustments
Despite keeping carbohydrates to a moderate amount (approximately 45 grams of carbs per meal using the plate method), you may find your blood sugars are still high 2 hours after meal. If this is the case, you may need to lower the carbohydrates at that meal and add a small snack in between meals. For example: instead of 45 grams of carbs per meal, drop to 30 grams or less and add a 15 gram carb snack in between meals.
Having smaller, more frequent meals/snacks can also be helpful if you’re struggling with morning sickness or acid reflux. For more tips on natural morning sickness relief, here’s an excellent article from Lily Nichols, RDN, CDE, CLT.
Satiety aka Fullness
It’s very common for women to feel extra hungry during their pregnancy. This makes sense because your body is using a lot of energy to grow a human being inside of you! However, since the bulk of our Standard American Diets (coincidence this spells SAD??) usually come from carbohydrates, the process of reducing carbohydrates in your diet may result in extra hunger.
To combat this extra hunger (without the added carbs) start to add more protein, healthy fats, and non-starchy vegetables to your meals. It is very important to have carbohydrates, protein, and fats at every meal to get the feeling of fullness that you expect after a meal.
A perfect example of this is a salad. If you’ve ever had a salad with all non-starchy vegetables and the tiniest bit of fat-free salad dressing possible, you were probably hungry an hour or two later. However, if you would have topped that base of dark leafy greens and non-starchy vegetables with a good quality, full-fat salad dressing, maybe some hemp seeds or nuts, and then added some protein such as ½ cup of beans, animal protein, or hard-boiled egg you would have felt a lot more full. The salad I just described has all three macronutrients: carbohydrates, proteins, and fats for satiety.
One Final Piece of Advice
If you have already been diagnosed with GD and spoke with your doctor, or even a dietitian, about your meal plan for your pregnancy, the information above may be a little different. That’s because conventional dietary recommendations during pregnancy state that a minimum of 175 grams of carbohydrates is necessary during pregnancy for normal growth and prevention of ketosis (which is often measured by an at-home urine test).
What I want to reassure you that you and your baby are still on track to a healthy pregnancy if you get less than 175 grams of carbohydrates per day. As I mentioned in part 1 of this series, the book Real Food for Gestational Diabetes is an excellent read to help you understand ALL THE SCIENCE to support today’s recommendations! Not all women need this excessive amount of carbs during pregnancy. Especially when insulin resistance is at the heart of GD.
For many women, consuming a minimum of 175 grams of carbohydrates per day sets them up to “fail diet therapy” and ultimately needing medication to control their blood sugars. There should be no shame or guilt if medication is needed, but it’s very frustrating for women to follow the advice of a professional and see no improvement or even get worse!
So where did this 175 grams of carbohydrates per day advice come from?
“You start with the Estimated Average Requirement for non-pregnant women of 100 g of carbohydrates per day. Then add 35g, to account for the increased energy demand of pregnancy (approximately 300 calories, divided by the recommended percentage of dietary carbohydrates of at least 45%, divided by 4 calories per gram of carbohydrate). Finally, you add 33 g, which is the amount of glucose estimated to be required by the fetal brain per day. Those numbers taken together, plus a little buffer (very scientific, right?), give us 175g per day.”1
However….the same committee also concluded:
“The lower limit of dietary carbohydrate compatible with life apparently is zero, provided that adequate amounts of protein and fat are consumed”.2
This statement negates the 100 grams of carbohydrates from the Estimated Average Requirement and leaves us with a minimum of 75 grams per day IN ADDITION to all the great nutrition from healthy sources of protein and fats. 75 grams per day is usually what’s described as a moderate-low carbohydrate diet.
A minimum of 75 grams of carbohydrates per day is NOT recommending a ketogenic diet during pregnancy! We still need some carbs in our diet, just not as many as we originally thought. Yes, this may result occasionally dipping into ketosis,a state of using fats for fuel instead of carbs, but it is temporary and perfectly safe in the presence of adequate calories from fats and protein. Urine testing for ketones is very different from your blood levels of ketones, making urine testing very inaccurate and in most cases, unnecessary.
If you want to learn even more about nutrition, medications, exercise, and myths surrounding GD, please check out Lily Nichols’ Real Food for Gestational Diabetes!
I hope you found this post helpful as you start to individualize your meal plan for GD or are looking to prevent GD. Please post any questions, comments, or stories in the comments section!
Click here to read Part 3 of my Gestational Diabetes Series: 3 Rarely Talked About Nutrients of Concern During Pregnancy.
References:
1 Nichols, Lily. Real Food for Gestational Diabetes. 2015.
2 Institute of Medicine (US). Panel on Macronutrients, and Institute of Medicine (US). Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Natl Academy Pr, 2005. Pg 275-277.
Follow me on social media and never miss a new post!
This post contains affiliate links, which means I receive a percentage of the sale if you use the link to make your purchase. This will not change the price of the product, but your support will help directly offsets the cost of web hosting and maintenance and is greatly appreciated!





Leave A Reply